In the 1990s, a few courageous scientists began to develop a technology that, for various reasons, was very difficult to believe in at the time: RNA vaccines. They overcame enormous technical hurdles and demonstrated that these vaccines worked in animals. The COVID-19 pandemic gave an unexpected boost to this new technology that would otherwise have taken much longer to mature, and the results were brilliant: in the first year of vaccination alone, COVID-19 vaccinations saved 20 million lives. Today, this technology is being extended to other disease fronts, demonstrating that gene-based techniques still have much to offer.

Since the Englishman Edward Jenner began testing his smallpox vaccine in 1796, following other pioneering work, an estimated 530 million people have been spared death from the disease. This is in addition to the countless millions of lives that other vaccines have saved and continue to save—up to five million a year, according to the World Health Organisation. Throughout history, different technical approaches have been used to prepare the body’s immune response to infection: first, attenuated or inactivated pathogens or fragments of them. Later, with the development of molecular biology, components of the pathogen could be produced in vitro, or recombinant vectors could be constructed, vehicles such as harmless viruses into which parts or genetic material of the pathogen are introduced.
The key: messenger RNA
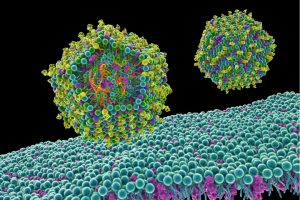
Viral vector vaccines are based on the idea that the body itself makes its own vaccine; it is given DNA from the virus that contains the gene for making some viral protein, or antigen. When the vaccinated person’s cells take up this DNA and use it to produce that protein, the immune system recognises it as foreign and triggers a response. A variant is the so-called DNA vaccine. The principle is similar, but instead of a viral vehicle, the DNA is delivered by other means, for example encapsulated in liposomes, tiny fatty vesicles. In both cases, an advantage of these strategies is that the production of the antigen in the cells themselves not only induces the production of antibodies, but also stimulates the other half of the immune system, the cellular response mediated by T-lymphocytes.
In the 1980s, researchers began experimenting with the option of introducing RNA into cells, initially with the aim of developing a form of gene therapy without genes. Gene therapy aims to correct a defective gene by providing a healthy version, particularly in the case of congenital diseases. The possibility of using messenger RNA, the disposable intermediate copied from DNA that translates genes into proteins, offered interesting additional advantages over the use of DNA: there was no need to introduce it into the cell nucleus, since RNA is translated in the cytoplasm, the part of the cell outside the nucleus; for the same reason, there was no risk of it getting integrated into the chromosomes with possible unwanted effects.
At the same time, it seemed an almost impossible undertaking: RNA degrades very easily, and it is also eliminated by the immune system as a foreign threat. At the beginning of this century, Hungarian biochemist Katalin Karikó and American immunologist Drew Weissman, together with other researchers, overcame these difficulties by wrapping RNA in lipid nanoparticles and modifying it so that it would not be destroyed.

RNA vaccine technology did not mature until the 2010s, although it had already shown its efficacy in laboratory animals. And it proved its worth during the pandemic. A key feature of these vaccines is that they can be rapidly adapted against any new pathogen simply by knowing its genome, which allowed the BioNTech-Pfizer and Moderna RNA vaccines against COVID-19 to be developed, tested and deployed in record time. The immense success of these vaccines and their contribution to the fight against the pandemic earned Karikó and Weissman the Nobel Prize in Physiology or Medicine in 2023.
From RNA to CRISPR
Since this milestone, which propelled and consolidated the technology, RNA vaccines have continued to be explored for other purposes: various infectious diseases such as seasonal flu, herpes, respiratory syncytial virus and others; gene therapy—their original purpose; vaccines against cancers as deadly as pancreatic cancer or melanoma; and even heart, neurodegenerative or bone diseases.

Advances in RNA as a therapeutic tool have also led to the emergence of a new field: RNA editing as an alternative to CRISPR. This genetic cut-and-paste system is making inroads into gene therapy, but it has potential drawbacks: modifying genes risks introducing changes in unwanted places in the genome. Instead, research groups are testing RNA editing, which, as a disposable intermediate in protein production, avoids the risk of permanent alterations. Three clinical trials have already been approved or are underway using this technology to treat two genetic diseases (alpha-1 antitrypsin deficiency and Stargardt disease) and the most common form of liver cancer, hepatocellular carcinoma.
What’s more, the ease and speed with which RNA-based drugs can be tailored to specific needs now makes these tools a great hope for personalised medicine, capable of producing, for example, cancer-specific drugs for individual patients. RNA medicine is only just beginning to realise its full potential.
Comments on this publication