The race to develop a vaccine against COVID-19 has broken every speed record in the history of immunisation. Until 2020, the vaccine that had completed all phases in the shortest time from virus sampling to final approval was the mumps vaccine, which took four years.
However, the global health emergency brought on by the massive outbreak of SARS-CoV-2 spurred research teams from across the globe to accelerate the process to create a viable vaccine in the shortest possible time without compromising safety. The result was the rollout of a vaccine in just eight months.
Considering this achievement, one wonders what impact it will have on the development of future vaccines or what techniques are currently being investigated to protect us from tomorrow’s viral threats. Here are four promising lines of research—which complement and reinforce one another—on which to focus our efforts to prevent future pandemics and to dream of even more exciting achievements:
1. Monitoring and sequencing of zoonotic pathogens
Of the 1.7 million unknown viruses estimated to exist in mammals and birds, almost half have the potential to infect humans. It would thus be prudent to get ahead of the game by doing genomic sequencing and monitoring of these zoonotic pathogens.
In contrast to classical vaccines that consist of inactivated or attenuated viruses, next-generation vaccines originate from the sequencing of genetic information that encodes a protein of the “invader.” Once a person is inoculated, the vaccine gains access to the host cell, where the antigenic genetic sequence is translated by the cellular machinery, which synthesises the protein and triggers an immune response to the invader.
Systematic sequencing of zoonotic pathogens would allow for the identification of key proteins or parts in the infection, and thus we could have already vaccine prototypes developed before other viruses like SARS-CoV-2 spill over to humans. Besides giving us a faster response time to a future pandemic, this would also enable the development of self- disseminating vaccines.
2. Self-disseminating vaccines
Ebola, H1N1, SARS, MERS, COVID-19… many of the most recent health emergencies, epidemic outbreaks and pandemics have been caused by zoonotic pathogens that have jumped to humans. Self-disseminating vaccines (also known self-spreading vaccines) are one of the best ways to eliminate these threats at source and prevent them from ever affecting our species.
Self-disseminating vaccines are able to spread autonomously through an animal population in two ways: transferable vaccines are administered on the fur of one or more individuals in populations of social species. These individuals act as spreaders among their fellow creatures who ingest the vaccine during the social act of grooming. The vaccine is not contagious from one animal to another, and only some individuals can spread it.
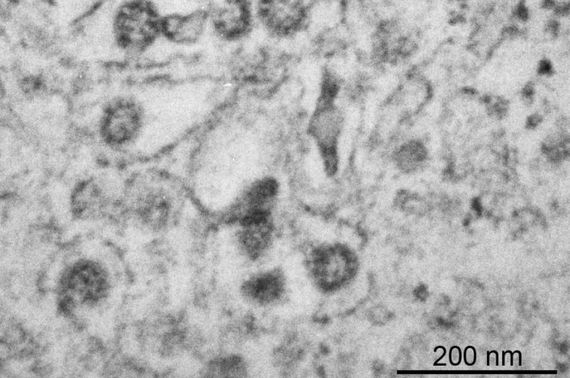
Transmissible vaccines, on the other hand, are contagious and are transmitted from one individual to another. These are genetically engineered vaccines in which a fragment of the pathogen’s DNA is introduced into a harmless virus that acts as a vector for transmission among the population. Upon infection, each newly infected animal acts as a potential transmitter.

Transferable vaccines have a range and spread limited to the vaccine load carried by “patient zero” and are therefore more controlled. Transmissible vaccines achieve a much greater and prolonged spread, but have so far only been shown to work in a minimally controlled scenario, and raise the possibility that the transmitting virus artificially introduced into the population may eventually evolve or jump to other species.
But if we are already able to develop such vaccines, why not (also) use them in people? Apart from the ethical considerations involved in deliberately infecting our fellow humans, there are two clear advantages for preferably using them in animals. First, there would be little point in developing an effective human vaccine against an animal virus if the virus mutates in its original environment and then re-emerges as a vaccine-resistant variant. Acting on the natural host of the virus means nipping the problem in the bud—eradicating the pathogen completely.
The other big advantage is that of shorter approval times, since by targeting an animal population the risks involved, such as the occurrence of certain side effects, are more manageable.
3. Food as a vaccine
One of the main limitations we face in the current pandemic is the unequal distribution of vaccines between developed and non-developed countries, exacerbated by the strict storage, preservation, transport and inoculation requirements that most synthesised vaccines require. In the short term, this is expected to be minimised by using Artificial Intelligence to optimise all the logistics associated with the distribution and delivery process.
In the medium term, an alternative that would facilitate the global distribution is that of vaccines inserted into foods. This is not a radically new idea, but rather a recycling of technologies and logistics that have already worked in a similar scenario: the use of genetically modified crops as a way to ensure access to essential nutrients, such as vitamin A in golden rice. In fact, edible vaccines for diseases such as polio are already in clinical trials with promising results.

The idea is to create a genetically modified food crop (a grain or plant) in whose genome the gene encoding an antigenic protein is inserted, so that the plant produces it and then accumulates it in its edible parts. Thus, when ingested, it is assimilated by the body and triggers the response of the immune system, which develops defences against future infections.
The advantages of edible vaccines are obvious: the antigenic proteins embedded within these cultures develop in the plant tissues in a much more stable form and can therefore be easily transported and stored. In addition, eating a vaccine is a non-invasive means of administration and does not require any medical assistance or equipment. Edible vaccines can be integrated into the most suitable crops for each region and, if necessary, each new harvest would produce them again, ensuring a regular supply.
These crops will not be the solution for an immediate response to an outbreak, but they can be used as a preventive vaccination campaign against chronic and/or endemic diseases.
4. Vaccines for chronic infectious diseases
In Africa over the past year, malaria has likely caused four times more deaths than COVID-19. This is both appalling and revealing. It shows that the great challenge in the field of vaccination today is to develop vaccines for chronic infectious diseases such as malaria, tuberculosis and AIDS, which cause countless deaths year after year.
The pathogens responsible for these types of infections are often much more complex (the parasite that causes malaria has more than 5000 genes compared to only 12 for the SARS-COV-2 virus), making it a Herculean task to identify the key proteins or regions to use to develop vaccines. Not only that, but they have evolved alongside humans over thousands of years and have developed sophisticated mechanisms to fool our immune systems.

But if the difficulty is daunting, so is the reward. Research in this area is a major driver in advancing new technologies for vaccine synthesis and treatments, including for autoimmune diseases. In fact, the vaccine developed by Oxford for COVID-19 was based on the development of an antimalarial vaccine.
Prevention, research and funding
The example of COVID-19 has highlighted the importance of protecting ourselves against unexpected biological threats. This time round, the speed of the research teams and high funding levels has meant that vaccines were available relatively quickly, but the threat of new global viruses makes it necessary to remain vigilant.
The most innovative techniques and advances in biotechnology and genetics, such as those discussed in this article, mean that a vaccine can be developed more quickly than just a few years ago, but the field of vaccine development is constantly evolving and will undoubtedly be a key sector in the medicine of the future.
Comments on this publication