For almost a year and a half, the world is facing the greatest epidemic battle of this century. The world is currently facing the greatest epidemic battle of this century. For years, the World Health Organization (WHO) has maintained a list of the pathogens that pose a real and present threat to humanity, and experts have long warned that the next great pandemic is not merely a science fiction plot. And yet, it now seems clear that we were not prepared. Even though it is not the most lethal virus we have encountered in recent times, the dizzying spread of the new coronavirus SARS-CoV-2 and the disease COVID-19 has provoked a major disruption of society and human activity on a planetary scale. Here we review what science knows about the virus and its disease, and what has already been achieved in the fight against this new scourge.
Interactive timeline: Science to Fight Coronavirus
[+] Watch Fullscreen
The origin of the virus
After a cluster of cases of pneumonia of unknown origin was detected in December 2019 and January 2020 in the Chinese city of Wuhan, in February 2020 three teams of Chinese researchers finally published all the details of the cause, a novel human coronavirus which the WHO provisionally called 2019-nCoV. The coronavirus, subsequently designated SARS-CoV-2 by the International Committee on Taxonomy of Viruses, is the seventh known human pathogen in this class. Four of them cause common colds, while the remaining two induce, respectively, Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS).

The analysis of its genome revealed that it is 79.6% identical to the SARS virus and 96% identical to bat coronaviruses, so it is assumed that it was transmitted from these animals to humans through another, as yet unconfirmed, species—pangolin was suggested as a suspect, but this has been questioned. The comparison of 93 genetic sequences of the virus indicates that it jumped to humans in November 2019. Chinese government research published in the South China Morning Post indicated that the first patient was a 55-year-old person in Hubei province who contracted the virus on November 17. Although the original outbreak was initially located in the Wuhan seafood market, there is no evidence of this place being the source.
In March 2021, the WHO published the report of its investigation in China that sought to clarify the origin of the virus. The findings were not particularly revelatory: the source was probably some animal species, not an escape from a laboratory, and it could not be confirmed whether the Wuhan market was the site of the first infections or just acted as an initial amplifier of the outbreak. Investigations are ongoing.
SARS-CoV-2 virus and its variants
Coronaviruses have been named as such since 1968 because under the electron microscope they appear surrounded by a barrier of rounded, crown-like projections, different from the sharp spikes of the flu virus. The envelope of the virus is formed by the Spike (S), Envelope (E) and Membrane (M) proteins, while in its interior is found the Nucleocapsid (N) protein together with its genome, a long single-stranded RNA with almost 30,000 bases.
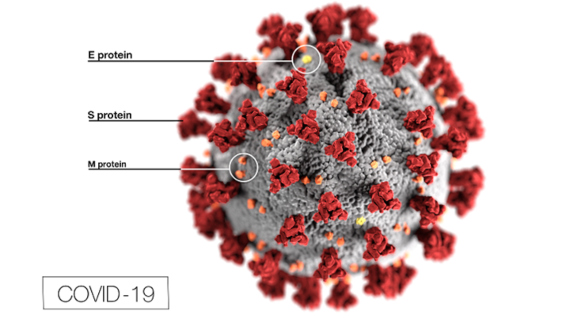
The S protein is the key that the virus uses to invade human cells, binding to a cell-surface protein called Angiotensin-Converting Enzyme 2 (ACE2), which is found mostly in the blood vessel cells of the heart and kidney, as well as in the epithelial cells of the lungs and intestine. The cell receptor is the same as that used by the SARS virus, but the S protein of the SARS-CoV-2 has been found to have 10-20 times more affinity for the ACE2 receptor than its SARS equivalent, which may partly explain its ease of spread. The high infectivity of the virus is facilitated by a peculiarity of its S protein, which is activated when a cellular enzyme called furin cleaves it in two during the process of invasion of the cell. This furin-cleaving sequence is not found in other human coronaviruses such as SARS, but is seen in other viruses such as influenza, HIV or Ebola; the presence of this trait is often associated with high infectious potential. Subsequently, other possible cellular receptors of the virus have been described.
In April 2021, more than one million genome sequences of SARS-CoV-2 were published on the Internet for use by researchers. In addition, although it is a slowly mutating virus, numerous variants have emerged during the first long year of the pandemic, some of them of particular concern because of their increased infectivity and in some cases greater virulence or resistance to current vaccines. B.1.1.7, first detected in the UK, has spread to become dominant in certain regions of the world, replacing the original Wuhan variant. Variant B.1.617 is partly responsible for a devastating escalation of infections in India in 2021.
Covid-19 contagion and disease
In February 2020, the WHO gave the name COVID-19 (COronaVIrus Disease 2019) to the illness caused by SARS-CoV-2, which had been previously announced in January as an outbreak of pneumonia of unknown cause in the Chinese city of Wuhan that initially affected 44 people. The patients exhibited fever, cough and breathing difficulties, and X-rays showed signs of pneumonia in some of them.

Although initially reported to be spread through small droplets expelled by coughing or sneezing, or through inanimate surfaces (fomites), there is now a broad scientific consensus that identifies aerosols as the main vehicle of transmission, while the disinfection of surfaces and objects is generally considered unnecessary and even harmful, as it may encourage the growth of resistant bacteria.
Studies indicate that the virus has an incubation period of approximately one week from infection to the appearance of symptoms, and that the window of infectivity also lasts about 7-8 days from the onset of the illness, or from a couple of days before. The basic virus replication number, R0 (the number of people on average infected by each patient in an equally mixed population with no previous contact with the pathogen), was initially estimated to be around 2.2, between 2 and 2.68, although it has varied widely by country and in some cases values of around 6 have been calculated. As for the severity of the illness, a large study in China showed that 80.9% of clinical cases were mild, with 13.8% having severe symptoms and 4.7% becoming critically ill. The illness is more serious in older people and those with previous pathologies, while children are less affected. The lethality of the virus among those infected (IFR) has been estimated at between 0.5% and 2% during the first wave of the pandemic, although above the age of 65 the risk of death is more than 1,000 times higher than for teenagers and 8,700 times higher in those over the age of 85.
However, there is also a large proportion of asymptomatic cases: one study suggested that 86% of those infected in Wuhan were not reflected in the data, while another put the total infected in that city at almost two million people, 19.1% of the population. More recent estimates put the proportion of asymptomatic infections at between 17% and 30%, although studies are ongoing.
Additional problems have emerged as the pandemic has progressed, such as multisystem inflammatory syndrome (MIS-C) in children, which in rare cases can be fatal, and the long-term persistence of various symptoms in many adults, which can include neurological conditions and cause disabling conditions. So-called persistent or long-term COVID, which preliminary data suggest may affect 10-30% of survivors of the infection, is still under investigation.
Diagnosis
Symptoms of COVID-19 are relatively non-specific, except for a few, such as the loss of smell, which is common and has been associated with the persistence of the virus in the olfactory epithelium. Otherwise, to confirm a possible clinical diagnosis of COVID-19, the use of tests has become standard throughout the world.
In January 2020, the WHO published the first protocols for genetic detection by Polymerase Chain Reaction (PCR) in respiratory mucosa or blood samples, followed by a test developed at the hospital Charité – Berlin University of Medicine, of which the WHO distributed 250,000 units to laboratories worldwide. Subsequently, new diagnostic kits have been created. PCR remains the gold standard for the confirmation of an infection, although antigen testing, which allows a patient’s infectivity to be assessed, has been used worldwide for mass screening. The first antibody screening was introduced in Singapore in February 2020, and serological tests are now widely used to identify people who have previously been infected.

Prevention and treatment and vaccines
Hundreds of clinical trials against COVID-19 have been undertaken throughout the pandemic and many are ongoing. However, there is still no specific and generally valid therapy, so patients receive mostly symptomatic treatment. The search is currently focused on antivirals, treatments for the hyperinflammatory syndrome caused by the virus, and antibodies, either from recovered human plasma or created in the laboratory, that can block the pathogen.
Steroids such as dexamethasone or hydrocortisone have shown the ability to reduce the risk of death by a third for patients on ventilators, while tocilizumab and sarilumab, two anti-inflammatory drugs, can also slightly reduce mortality. The antiviral remdesivir has been widely administered according to data suggesting a reduction in hospitalisation time, but its efficacy has been questioned by the results of a large WHO trial.
Much more successful has been the roll-out of vaccines. Hundreds of them are in various stages of development, testing or approval, and as many as 13 different formulations are already being administered under emergency authorisations in different countries. These include inactivated virus vaccines (Sinovac and Sinopharm), recombinant adenoviral vectors (AstraZeneza/Oxford, Janssen, Gamaleya-Sputnik, CanSino) or RNA vaccines (Pfizer/BioNTech, Moderna). Vaccination is progressing worldwide with encouraging results, although much more slowly in developing countries.
For the rest, the battle against the virus is largely focused on non-drug interventions, notably the use of face masks, travel restrictions, lockdowns, social distancing, contact tracing, isolation of confirmed cases and quarantines. These measures have been applied unevenly in different countries.
Comments on this publication