The pandemic of SARS-CoV-2, the coronavirus which causes COVID-19, looks like a sinister lottery: many people get over the infection without symptoms or with minor discomfort, while others die. From the beginning, age and prior illnesses have emerged as risk factors, something common in other infections such as the flu. But a percentage of young and healthy people also succumb to the virus, and even children have fallen seriously ill, though this is rare. Knowing more about the risk factors will enable the identification of those patients with whom precautions must be taken and therapeutic efforts made, as well as alleviating some of the panic surrounding the pandemic.
With the first news of a new pneumonia in Wuhan, China, came a snapshot of the people most at risk of becoming seriously ill and dying. In January, the first studies with small groups of patients were published: older men with problems of diabetes, hypertension, cardiovascular or respiratory disease were the most likely to succumb. Later studies with older populations have corroborated these conclusions. However, why are people dying from COVID-19 who aren’t elderly or don’t have previous illnesses?
As summarized for Bloomberg by infectious disease experts Arturo Casadevall at Johns Hopkins University and Liise-anne Pirofski at the Albert Einstein College of Medicine (USA), a complex tableau of variables can determine what our fate will be in the event of infection: the amount of virus we receive, the route by which it enters the body, the specific variety of virus, our genes and our clinical and immunological history can tip the balance towards any position between the two extremes: an asymptomatic infection or death.
However, Casadevall explains to OpenMind that there is a high degree of uncertainty in these variables: “Chance probably makes a huge contribution to outcome when it comes to the size of the infective inoculum, the site of initial infection and even the time of day that infection occurs – given diurnal rhythms.” From the first of these factors, the question arises: Has the relationship between the amount of virus received and the progression of the disease been demonstrated?
Dose at inoculation and severity
“As far as I know, a link between dose at inoculation and severity has not been reported at this point for SARS-CoV-2/COVID-19,” microbiologist Marta Gaglia at Tufts University (USA) told OpenMind. Gaglia adds that even with other better-known viruses such as influenza, it is difficult to extrapolate the results of animal experiments to human-to-human infections. “One confounding factor is that it is likely that if you are exposed to more virus, you are generally more likely to get productively infected in the first place and thus developing disease at all.”
It is also unclear how the route of infection influences the course of COVID-19, but experts suggest that the region of the body that the virus succeeds in conquering may be decisive. As Stanley Perlman, an immunologist specializing in coronaviruses at the University of Iowa (USA), explained in Nature, when SARS-CoV-2 manages to descend from the nose or throat into the lungs, it is probably as lethal as the coronavirus of the Severe Acute Respiratory Syndrome (SARS), which kills one in ten infected people. Perlman has told OpenMind that a more severe clinical presentation is likely to trigger a stronger immune response, but this also doesn’t necessarily define the subsequent course of the illness.
In fact, the immunology of the virus is still another major unknown: the immune system fights the infection, but in some cases an immune overreaction, or Cytokine Release Syndrome, is observed, which may be the direct cause of death. This “cytokine storm” may also lead to the formation of blood clots, a potentially lethal symptom seen in 20-30% of the most severe patients. However, blood clotting could also be related to pathologies such as hypertension, diabetes or even old age itself. Interestingly, it has been observed that the most devastating effects of COVID-19 seem to respect patients who are immunosuppressed, either by disease or treatment. In contrast, a rare hyper-inflammatory syndrome appears to be behind a small number of cases of deaths in children.
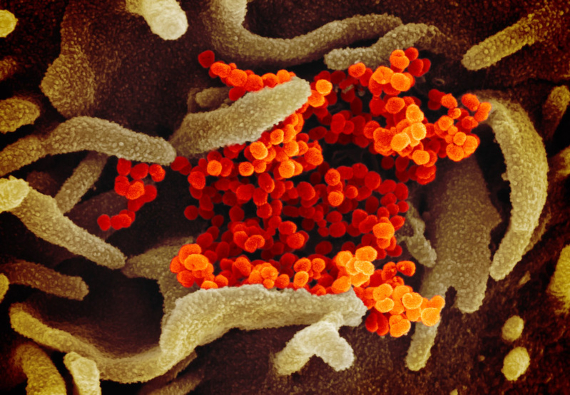
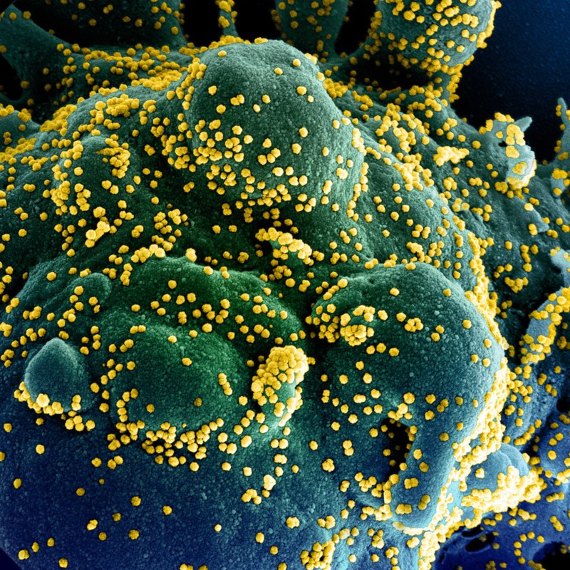
The virus’ main cellular receptor
Another question still under debate is whether different forms of the virus can be linked to more serious infections. Recently, a preprint (study not yet reviewed or published) found that a form of the virus with a point mutation in its Spike protein, which interacts with the cell receptor, had spread preferentially in Europe and the USA. The authors speculated on the possibility that this mutated version might be more transmissible than the original form from Wuhan, but did not prove it to be the case. In addition, the study acknowledged that the mutation “did not predict hospitalization.” Various experts have clarified that currently we cannot talk about different strains of the virus, since there is no evidence of a change in its biological properties.

Finally, an essential question is whether there are alleles —gene variants— even associated with ethnic groups, which could worsen the prognosis. One focus of attention for researchers is the virus’ main cellular receptor, the ACE2 (Angiotensin-Converting Enzyme 2) protein. Since ACE2 is also involved in the regulation of blood pressure, one of the risk factors, it is imperative to find out if different variants or levels of expression of this receptor can influence the evolution of COVID-19.
“ACE2 expression is higher in many of the high-risk groups,” virologist Jeremy Rossman, from the University of Kent (United Kingdom), told OpenMind. “There are also variants of ACE2 that affect the amount of ACE2 on the cell surface and the geographic distribution somewhat reflects areas that have been hardest hit by the virus.” Rossman adds that not only could the amount of ACE2 affect the replication of the virus and therefore the disease, but conversely, the coronavirus also appears to alter the levels of expression of its receptor in the cells, so specifying the role of this protein in determining the severity of the disease will be complicated. “All we really have on ACE2 right now is questions,” he concludes.
The deaths of men outnumber those of women
At the same time, numerous research groups are addressing the issue of susceptibility genes from a broader, genome-wide approach. From Rockefeller University (USA), infection geneticist Jean-Laurent Casanova is co-leading the international consortium COVID Human Genetic Effort to discover variants in immunity genes that may aggravate the course of COVID-19 or, conversely, confer resistance. “The genes whose mutations underlie severe influenza or other viral pneumonia pneumonias are good candidate genes,” Casanova told OpenMind. Similarly, the COVID-19 Host Genetics Initiative project is trying to find genetic determinants. But among these possibilities, there is one more obvious factor that stands out: the deaths of men outnumber those of women. The question as to whether hormone levels might play a role is under debate, but it has been suggested that the double X chromosome in women might benefit them by providing an extra copy of certain immunity genes.
For his part, Casadevall is pessimistic about discovering a handful of specific genes that could be decisively linked to the final expression of COVID-19 in each patient. “This is a disease for which multiple organ systems are involved and that means that thousands of genes are involved in the response, which in turn means that for most people the contribution of any one genetic marker is likely to be small,” he says. “I realize that this is not what people want to hear as most would like a simple answer.”
While research into the risk factors continues, data analysis helps locate biomarkers that can predict a more serious prognosis. An Artificial Intelligence system used by scientists at Huazhong University of Science and Technology in Wuhan has selected three markers that predict mortality more than 10 days in advance in more than 90% of cases: the enzyme lactic dehydrogenase (LDH, a sign of tissue damage), C-reactive protein (hs-CRP, an indicator of inflammation) and the lymphocyte count. Another team from New York University has located three other markers that predict with 70-80% accuracy who will become extremely sick: elevated levels of the liver enzyme alanine transaminase (ALT), high levels of haemoglobin, and body aches. Other research is taking a similar approach, looking for tools that will allow doctors to identify the most susceptible patients early in order to take quick and decisive actions to avoid a fatal outcome.
Comments on this publication