Making human organs and tissues in the laboratory that function identically to the original ones has long ceased to be a fantasy. The bioengineering of tissues and organs, based on the use of stem cells and their derivative techniques, has made astonishing progress in recent years. Although widespread clinical applications will not be immediate, the basic technology needed to create healthy replacement tissues to repair diseased organs is already a reality today. And while we wait for the promises of the new regenerative medicine, whose most recent achievements we review here, to reach our local hospital, researchers are already exploiting the enormous power of organoids—miniature versions of real organs in a culture dish—to study how they work and to test new drugs and therapies tailored to the cells of each patient.
Digestive organs
A handful of human stem cells helped researchers at Cincinnati Children’s Hospital Medical Center to create a miniature version of a stomach in 2014. James Wells, an expert in developmental biology and endocrinology and co-leader of the research says proudly: “We’ve discovered how to promote the formation of three-dimensional gastric tissue with a complex composition and cellular structure.” The key lies in replicating in culture plates the exact steps in the formation of the stomach during embryonic development, which were used as an instruction book.
In addition to their possible future uses for repairing diseased stomachs, the organoids made by these bioengineers are ideal for investigating in detail how the infection caused by the bacteria Helicobacter pylori, which is responsible for peptic ulcers, evolves in real time, or for analysing how obesity affects the functioning of this organ, among other possible applications.

Wells and his collaborators have recently perfected their stomach organoids, endowing them with glands and neurons that control muscle contraction. “We can now assemble complex organ tissues from separately derived components, similar to an assembly line approach,” he says. The same technique has been used to create organoids of other segments of the digestive tract, such as the oesophagus or a miniature intestine with villi that absorb nutrients like the real organ. In an even more spectacular breakthrough, collaborative work with bioengineer Takanori Takebe has produced a system of three interconnected organoids: liver, pancreas and bile ducts.
Vocal cords
In November 2015, scientists at the University of Wisconsin-Madison announced a major achievement: they had successfully grown human vocal cord tissue in the laboratory that could restore the voice of individuals who have lost their vocal cords to cancer or other pathologies. “Our vocal cords are made up of special tissue that has to be flexible enough to vibrate, yet strong enough to bang together hundreds of times per second,” explained Nathan Welham, director of the work. “It’s an exquisite system and a hard thing to replicate,” he admitted. Welham and his team isolated vocal cord cells from a cadaver and grew them on a 3D collagen scaffold. Within two weeks, the cells formed a vocal cord structure that vibrated identically to the original.

However, building vocal cords capable of withstanding the stresses this organ undergoes is still a challenge. Another team at the University of Wisconsin-Madison led by Susan Thibeault has succeeded in creating vocal fold mucosa that responds just like natural mucosa to stresses such as tobacco smoke. Meanwhile, at McGill University in Canada, a group of scientists has produced a biological hydrogel that could be used to strengthen this tissue and help it withstand the mechanical stress it is subjected to.
Ovaries, vagina and penis
Hormonal problems suffered by women who have had their ovaries removed, who are affected by cancer or who are entering menopause could be alleviated by tissue engineering. Scientists at the Wake Forest Institute for Regenerative Medicine created rat ovarian tissue in microcapsules that simulate the organ’s natural structure. “A bio-artificial ovary that naturally releases sex hormones like estrogen and progesterone is better than supplying these types of hormones artificially,” explained Emmanuel C. Opara, who led the research. Opara’s team then found that transplanting these tissues into rats replaced the lost hormone function. Other groups are creating ovarian organoids from women with cancer, allowing them to test treatments and find the best one for each patient before administering them.
At the same institute, Anthony Atala and his team transplanted for the first time into four teenagers with vaginal aplasia—a malformation disorder—vaginal tissue grown in the laboratory from their own cells, previously extracted in a biopsy. The cells were grown on a biodegradable vagina-shaped scaffold custom-made for each patient, which the surgeons implanted after six weeks of growing in culture. Once the tissue was implanted, new nerves and blood vessels began to form spontaneously around it, and the new organ integrated with the rest of the reproductive system. Atala has also experimented with the manufacture of bioengineered penises, which have worked successfully in rabbits.
Muscle
Muscle is an obvious target for laboratory tissue generation, as it is not as complex in structure as some organs. Even so, it is necessary to achieve the right tissue configuration to allow it to perform its function. Various research groups have cultured muscle precursor cells, arranging them on different types of artificial matrices so that they can align and work together as muscle fibres. These laboratory muscles are being used to study muscle ageing and regeneration. As in the case of other in vitro cultured tissues, one of their main uses is to test new drugs to see how human muscle would react in vivo, which will be used to design new personalised treatments in the field of precision medicine.

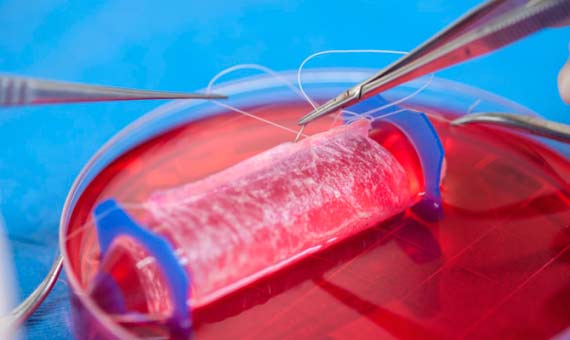
Blood vessels
The creation of blood vessels in culture has been one of the main lines of research since the birth of tissue engineering. As early as 1986, the first successes were achieved with the fabrication of natural-like blood vessels using collagen, smooth muscle, fibroblasts and endothelial cells that line the inside of the tube. To obtain the right structure, researchers are testing different strategies, such as using a scaffold of biological polymers to support the cells. These compounds are biodegradable, so that once implanted they are replaced by the body’s own tissue, resulting in a fully functioning, natural blood vessel. Another possibility is to create tubes of biological material in cell cultures, with the cells washed away before implantation in the patient, so that the body’s own cells complete the work through a normal healing process.

Heart
In the early decades of regenerative medicine, the heart was also the focus of much research, because of the great benefits these advances could bring to cardiovascular patients. Progress in culturing heart muscle came early, but another much more complicated challenge is to grow a complete and functional heart. This was successfully achieved in 2008 by researchers at the University of Minnesota’s Center for Cardiovascular Repair. They used a process called decellularization, which involves taking a heart—they experimented using pigs and rats—and removing the cells present to keep only the structure, “nature’s platform” in the words of the researchers. They then reseeded that natural scaffold with a mixture of progenitor cells to recreate the living tissue. Four days after incorporating the cells, contractions were already visible in some areas. And after eight more days the hearts were beating.
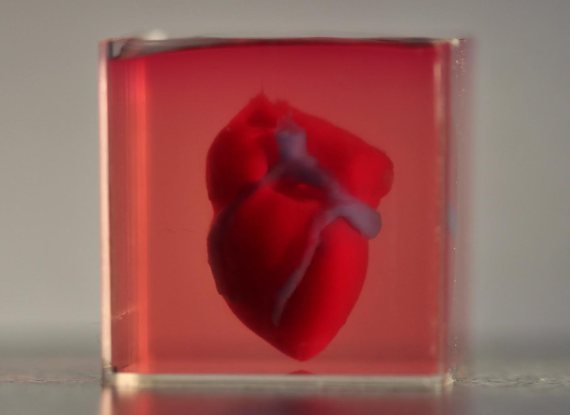
In 2019, researchers at Tel Aviv University created the first complete human heart—albeit the size of a rabbit’s—through 3D bioprinting using a patient’s cells and biological materials to create the supporting structure. Using stem cells, other groups have generated sesame-seed-sized cardiac organoids that organise themselves without the need for scaffolding, with all their cell types and internal chambers, and within days in culture begin to beat. In 2020, the first transplantation of lab-grown heart muscle into a human patient with a heart condition was carried out in Japan in the first phase of a clinical trial.
Neurons
Recreating nerve tissue is perhaps the most ambitious goal of tissue bioengineering, both because of the special complexity of neural connections and because of the advances that could be made in the fight against neurodegenerative diseases and other pathologies. In 2014, scientists at Tufts University created the first complex three-dimensional model of the cerebral cortex of a rat with biochemical and electrical responses similar to those of a real brain. Although not a complete brain, the artificial replica copies the natural structure of grey matter (the cell bodies of neurons) and white matter (the axons of neurons). The neurons are arranged in concentric rings simulating the formation of layers in the brain. The 3D model, which can survive for more than two months, will be useful for studying brain function in vivo, as well as the effects of drugs on neurons and the diseases that affect them.

In recent years, research teams have created increasingly sophisticated brain organoids. These mini-brains in a culture dish go so far as to make their own blood vessels and establish neural connections capable of transmitting impulses similar to the real brain waves recorded during foetal development. For Johns Hopkins University scientist Thomas Hartung, one of the pioneers of this technology, although this mini-brain activity is purely mechanical, in some ways it is akin to a primitive type of thinking. In 2021, a study led by the Heinrich Heine University in Düsseldorf produced brain organoids that created their own optic vesicles, the structures that give rise to eyes. Although very rudimentary, they possessed distinct parts emulating the cornea, lens and retina, along with functional neurons, and responded to light with electrical activity. Eyes are also being recreated in organoid form.
However, it should be made clear that scientists are not trying to develop a thinking brain on a plate, which is still infinitely far from today’s technologies. Instead, brain organoids are invaluable tools for investigating the development of the nervous system, its diseases and possible treatments. In another recent breakthrough, human mini-brains have been transplanted into the brains of mice, which will allow in vivo models of human neurological diseases to be obtained that are much closer to reality than those currently used.
Elena Sanz / Javier Yanes
Comments on this publication